Uterine Cancer
Uterine cancer, also known as endometrial cancer, begins in the lining of the uterus and is the most common gynecological cancer. It typically affects postmenopausal women, although it can occur at any age. Early detection through abnormal uterine bleeding can lead to successful treatment. At Burjeel Cancer Institute, we provide comprehensive care for uterine cancer, offering a range of treatments including surgery, radiation therapy, and chemotherapy, with a focus on personalized, patient-centered care
Common Symptoms of Uterine
- Abnormal vaginal bleeding or discharge (particularly after menopause)
- Pelvic pain or discomfort
- Pain during intercourse
- Unexplained weight loss
- Frequent urination
Risk Factors for Uterine
Age
Uterine cancer is most common in women over 50.
Hormone Therapy
Prolonged use of estrogen without progesterone increases the risk of endometrial cancer.
Obesity
Excess body fat increases estrogen levels, raising the risk of uterine cancer.
Family History
A family history of uterine cancer or genetic syndromes like Lynch syndrome increases risk.
Never Being Pregnant
Women who have never been pregnant have a higher risk of developing uterine cancer.
Diabetes
Women with diabetes are more likely to develop uterine cancer.
Tamoxifen Use
Long-term use of tamoxifen, a drug used to treat breast cancer, can increase the risk.
Diagnostic Procedures
Early and accurate diagnosis of uterine cancer is key to successful treatment. We offer advanced diagnostic techniques, including
Pelvic Exam
A routine pelvic exam helps detect abnormalities in the uterus and surrounding structures.
Transvaginal Ultrasound (TVUS)
A detailed imaging test used to visualize the uterus and detect abnormalities in the endometrium.
Endometrial Biopsy
A small sample of the endometrial tissue is taken and analyzed to check for the presence of cancer cells.
Dilation and Curettage (D&C)
A procedure used to remove tissue from the uterus for further examination if the biopsy is inconclusive.
CT Scan and MRI
Imaging studies used to determine the extent of cancer spread within the pelvis or to other parts of the body.
PET-CT Scan
Used to detect metastatic spread of cancer throughout the body, particularly in advanced cases.
Genetic Testing
For patients with a family history of endometrial cancer or Lynch syndrome, genetic testing may be recommended.
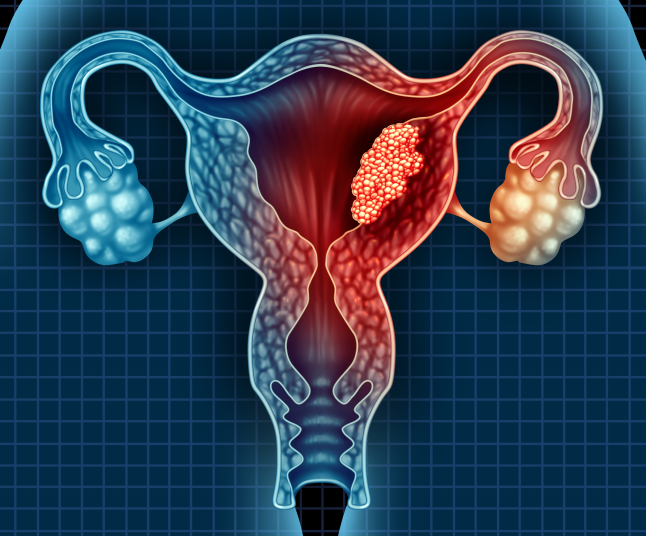
Treatment Options
Chemotherapy and Medical Oncology
- Systemic Chemotherapy: Often used in advanced stages of uterine cancer or when cancer has spread beyond the uterus, chemotherapy works to destroy cancer cells throughout the body.
- Combination Chemotherapy: Multiple chemotherapy drugs may be used together to increase treatment effectiveness, often combined with surgery or radiation.
Hormone Therapy
- Progestin Therapy: Hormone therapy may be used to slow the growth of uterine cancer cells, particularly in women with early-stage cancer who wish to preserve fertility.
- Estrogen Blockers: Hormone therapies that block the effects of estrogen can be used for hormone-sensitive uterine cancers.
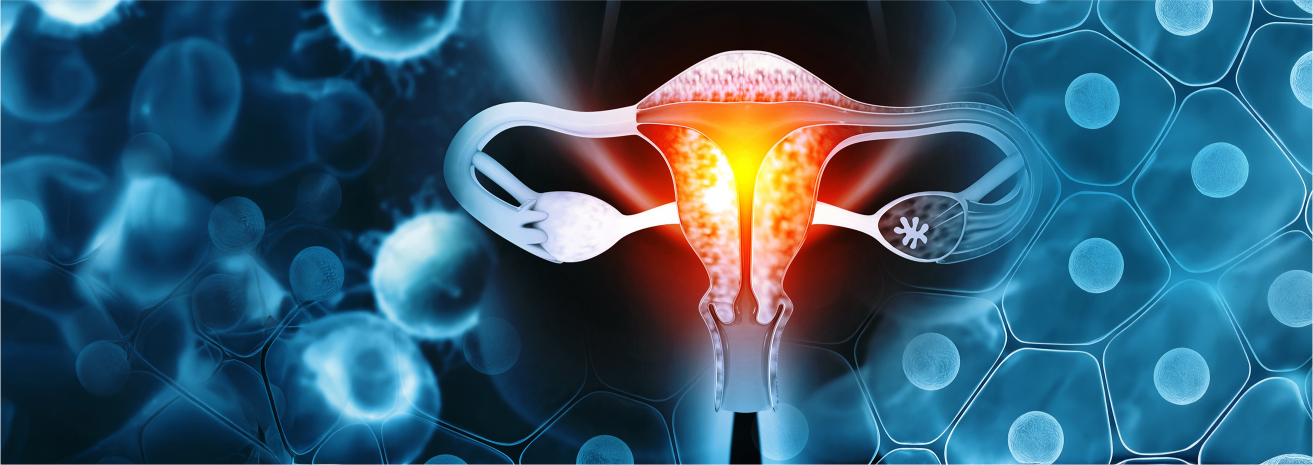
Radiation Therapy
- External Beam Radiation Therapy (EBRT): Radiation is delivered to the pelvis to kill cancer cells and reduce tumor size.
- Brachytherapy: Internal radiation therapy where radioactive materials are placed inside the uterus, allowing for precise targeting of cancer cells.
Surgical Treatment
- Total Hysterectomy: The most common treatment for uterine cancer, involving the removal of the uterus, along with the cervix, ovaries, and fallopian tubes in some cases.
- Bilateral Salpingo-Oophorectomy: Removal of both ovaries and fallopian tubes, often performed in combination with a hysterectomy for patients with higher-stage cancer.
- Lymph Node Dissection: Removal of nearby lymph nodes to check for the spread of cancer.
- Minimally Invasive Surgery: Laparoscopic or robotic-assisted surgery options offer smaller incisions, less pain, and faster recovery times.
Multidisciplinary Approach
Uterine cancer treatment requires collaboration among a wide range of specialists, including
- Gynecologic Oncologists
- Medical Oncologists
- Radiation Oncologists
- Surgical Oncologists
- Radiologists
- Pathologists
- Genetic Counselors
- Oncology Nurses
- Palliative Care Specialists
This multidisciplinary team works together to develop a personalized treatment plan for each patient based on the stage and characteristics of the cancer
Supportive Care and Patient Services
We provide a variety of supportive care services to help women with uterine cancer manage their treatment and improve their quality of life
Nutritional Counseling
Personalized dietary advice to help manage side effects and maintain strength during treatment.
Fertility Preservation
For women who wish to preserve their fertility, we offer options such as egg freezing before treatment begins.
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic uterine cancer.
Psychosocial Support
Counseling services to help patients and their families cope with the emotional and psychological challenges of a uterine cancer diagnosis.
Physical Rehabilitation
Post-surgical rehabilitation to help patients regain strength and function after surgery.
Survivorship Program
Ongoing care and support for women who have completed treatment, focusing on long-term health and recurrence prevention.
Patient Journey
We guide uterine cancer patients through every step of their journey, from diagnosis to recovery
Initial Consultation
A thorough evaluation with the gynecologic oncology team, including diagnostic imaging and tests to assess the extent of the disease.
Personalized Treatment Plan
A customized treatment plan is developed based on the patient’s diagnosis, cancer stage, and overall health.
Treatment and Support
Patients receive comprehensive care, supported by our multidisciplinary team and personalized supportive care services.
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor their recovery, assess treatment response, and manage long-term health.







