Prostate Cancer
Prostate cancer is one of the most common cancers in men, particularly those over the age of 50. While many cases are slow-growing and may not cause significant health problems, some prostate cancers can be aggressive and require immediate treatment. At Burjeel Cancer Institute, we offer comprehensive care for prostate cancer, including early detection, advanced diagnostic tools, and cutting-edge treatments tailored to each patient’s unique condition and needs.
Symptoms and Risk Factors
- Difficulty starting or maintaining urination
- Weak or interrupted urine flow
- Frequent urination, especially at night
- Blood in the urine or semen
- Pain or discomfort in the pelvic area or lower back
- Erectile dysfunction.
Risk Factors for prostate cancer include
Age
The risk increases significantly after the age of 50.
Family History
A family history of prostate cancer increases the risk, especially if close relatives have been diagnosed.
Race
African-American men have a higher risk of developing prostate cancer and tend to have more aggressive forms of the disease.
Genetic Mutations
Certain inherited gene mutations, such as BRCA1 and BRCA2, may increase the risk.
Diet and Lifestyle
A diet high in fat and low in fruits and vegetables may contribute to prostate cancer risk.
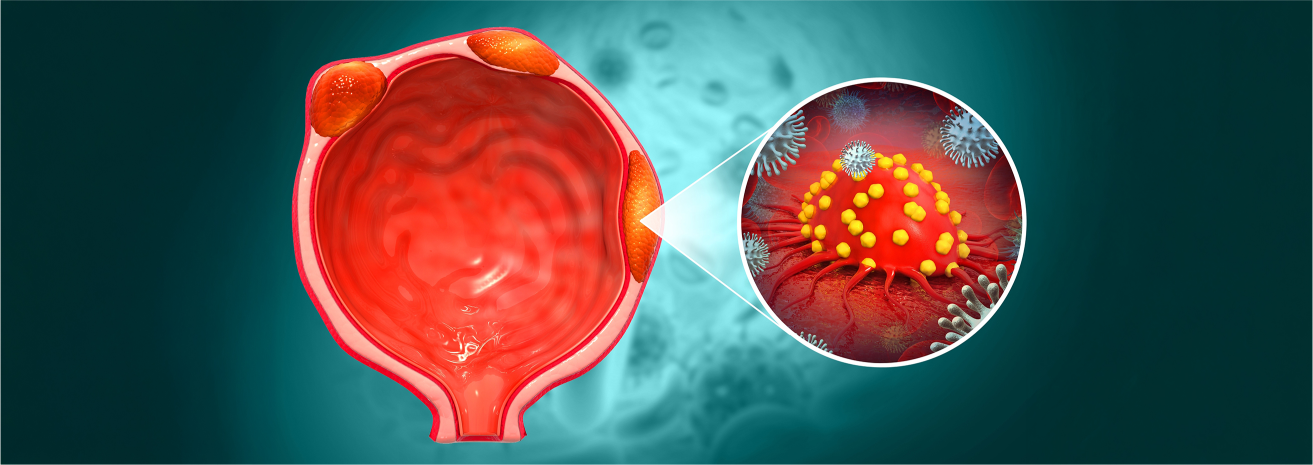
Diagnostic Procedures
To diagnose prostate cancer accurately and determine the best treatment, we offer a range of advanced diagnostic tools, including
Prostate-Specific Antigen (PSA) Test
A blood test that measures the level of PSA, a protein produced by the prostate gland. Elevated levels may indicate prostate cancer.
Digital Rectal Exam (DRE)
A physical examination where a doctor checks the prostate for abnormalities.
MRI Fusion Biopsy
Combines MRI imaging with a traditional biopsy to precisely target suspicious areas of the prostate.
Transrectal Ultrasound (TRUS)
An ultrasound probe is inserted into the rectum to provide detailed images of the prostate.
PET-CT and Bone Scans
Used to determine if the cancer has spread to the bones or other parts of the body.
Genomic Testing
Genetic testing to identify specific mutations that can guide treatment, such as BRCA mutations or other relevant biomarkers.
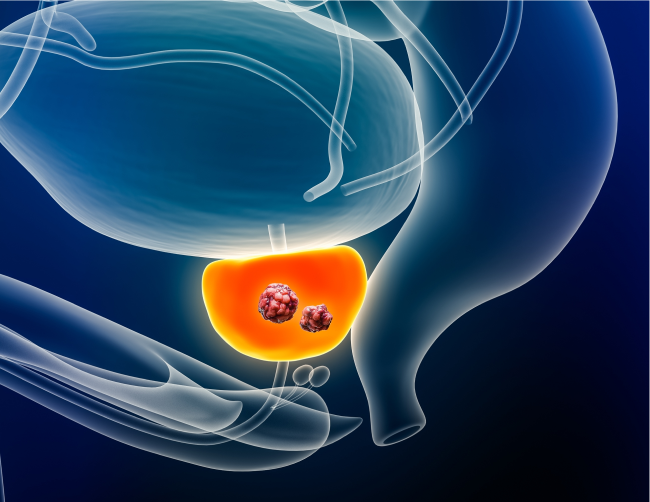
Treatment Options
Targeted Therapy and Immunotherapy
- PARP Inhibitors: Used for patients with BRCA mutations, these drugs target and destroy cancer cells by interfering with their ability to repair DNA.
- Immunotherapy (Sipuleucel-T): A type of therapy that trains the immune system to attack prostate cancer cells, used in advanced cases.
Chemotherapy and Medical Oncology
- Chemotherapy: Often used in advanced or metastatic prostate cancer, chemotherapy works by destroying rapidly dividing cancer cells.
- Hormone Therapy: Also known as androgen deprivation therapy (ADT), this treatment reduces or blocks the body’s production of male hormones, which can fuel the growth of prostate cancer.
- Oral Medications: Drugs such as abiraterone and enzalutamide block the effects of testosterone on prostate cancer cells
Radiation Therapy
- External Beam Radiation Therapy (EBRT): Delivers high-energy rays to the prostate, destroying cancer cells while sparing healthy tissues.
- Brachytherapy (Internal Radiation): Radioactive seeds are implanted directly into the prostate to deliver targeted radiation over time.
Surgical Treatment
- Radical Prostatectomy: Removal of the entire prostate gland, often used in cases of localized prostate cancer.
- Robotic-Assisted Laparoscopic Surgery: A minimally invasive approach that allows for precise removal of the prostate with faster recovery and less post-operative pain.
- Transurethral Resection of the Prostate (TURP): Used to treat prostate cancer symptoms, particularly when there are urinary problems.
Multidisciplinary Approach
Prostate cancer care involves a team of specialists who collaborate to provide personalized treatment plans for each patient. The team includes
- Urologic Surgeons.
- Medical Oncologists.
- Radiation Oncologists.
- Radiologists.
- Pathologists.
- Genetic Counselors.
- Oncology Nurses.
- Palliative Care Specialists.
This multidisciplinary team ensures that every aspect of a patient’s care is considered, from diagnosis to treatment and beyond.
Supportive Care and Patient Services
We offer a wide range of supportive care services to help prostate cancer patients manage their treatment and maintain their quality of life
Nutritional Counseling
Specialized dietary plans to support overall health during prostate cancer treatment.
Physical Rehabilitation
Post-surgical rehabilitation to help men regain strength and function after prostate cancer surgery.
Psychosocial Support
Counseling services for patients and families coping with the emotional and psychological challenges of a prostate cancer diagnosis.
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic prostate cancer.
Sexual Health Counseling
Support and guidance for managing sexual health issues related to prostate cancer treatment.
Patient Journey
We guide prostate cancer patients through every step of their journey, from diagnosis to recovery.
Initial Consultation
A comprehensive evaluation with our prostate cancer care team, including diagnostic imaging and tests to assess the cancer’s stage.
Personalized Treatment Plan
Based on the patient’s diagnosis, we develop a customized treatment plan that may include surgery, radiation, hormone therapy, or other approaches.
Treatment and Support
Patients undergo the recommended treatments, supported by our multidisciplinary team of specialists and supportive care services.
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor for recurrence and manage long-term health, including screenings, imaging, and lifestyle support.







