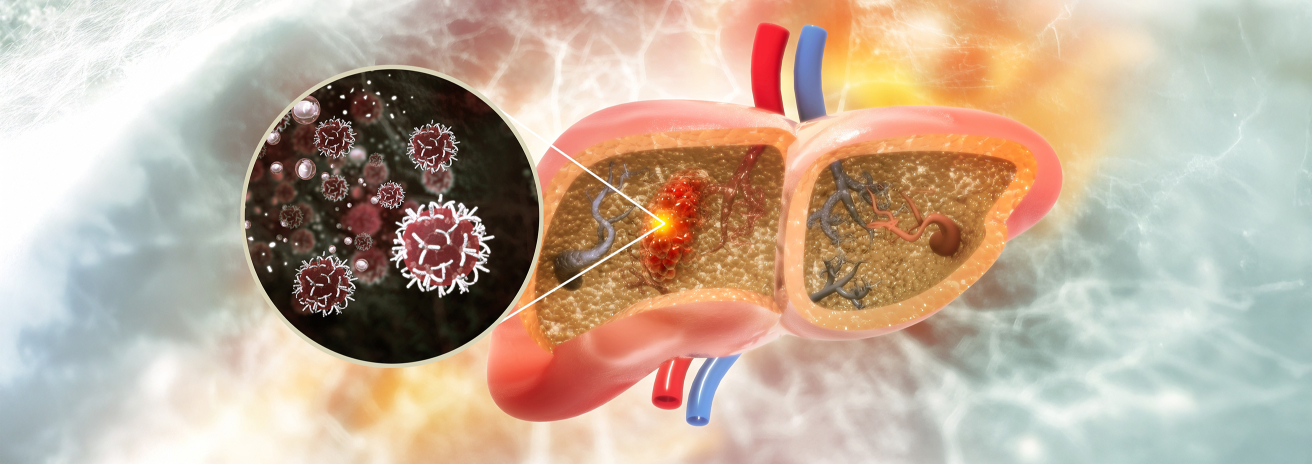
Liver Cancer
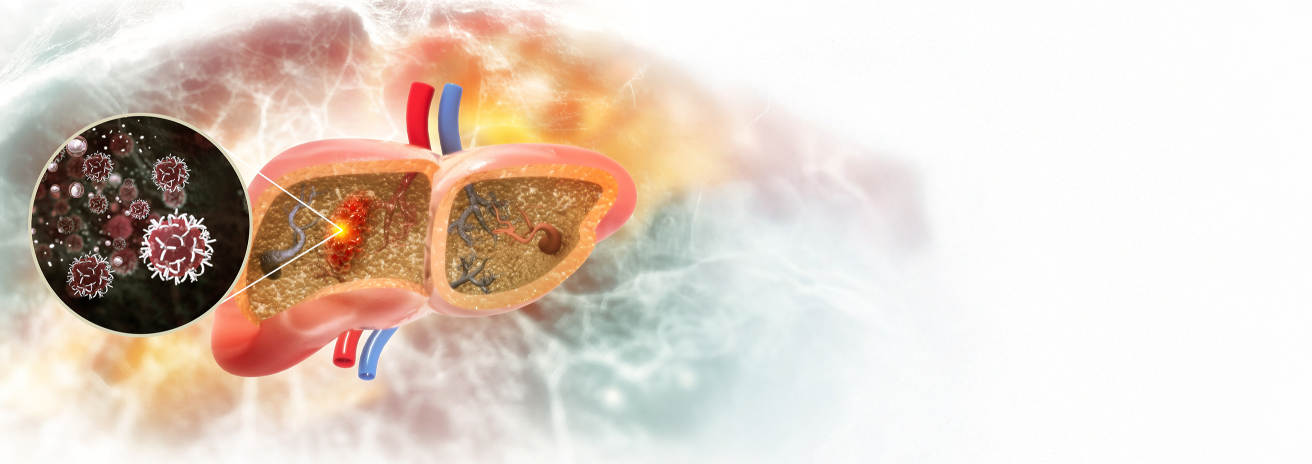
Liver cancer, also known as hepatocellular carcinoma (HCC), is the most common type of primary liver cancer, usually developing in people with chronic liver disease or cirrhosis. The liver is also a common site for metastatic cancer, where cancer cells from other organs spread to the liver. Early detection is critical for effective treatment, and at Burjeel Cancer Institute, we offer comprehensive care for liver cancer through advanced diagnostic tools, surgery, targeted therapies, and liver transplantation options
Symptoms and Risk Factors
- Unexplained weight loss
- Loss of appetite
- Upper abdominal pain or discomfort
- Swelling or bloating in the abdomen
- Jaundice (yellowing of the skin and eyes)
- Nausea and vomiting
- Fatigue and weakness
- Dark-colored urine or pale stools
Risk Factors for Liver Cancer
Chronic Hepatitis B or C Infections
Long-term infection with hepatitis B or C viruses significantly increases the risk of liver cancer.
Cirrhosis
Scarring of the liver due to alcohol abuse, fatty liver disease, or chronic hepatitis infections increases the risk.
Alcohol Consumption
Heavy and long-term alcohol use can lead to liver damage and cirrhosis, a major risk factor for liver cancer.
Non-Alcoholic Fatty Liver Disease (NAFLD)
This condition, which often occurs in obese individuals or those with type 2 diabetes, can progress to cirrhosis and increase the risk of liver cancer.
Aflatoxin Exposure
Exposure to aflatoxins (toxins produced by mold) found in improperly stored food increases the risk.
Family History
A family history of liver cancer may increase your risk of developing the disease.
Diagnostic Procedures
We use state-of-the-art diagnostic tools to detect and stage liver cancer, including
Ultrasound
Often used as a first-line screening tool to detect liver masses.
Liver Biopsy
A tissue sample is taken from the liver for analysis to confirm the presence of cancer.
CT Scan
Provides detailed cross-sectional images of the liver, helping to locate and stage liver cancer.
MRI with Contrast
Offers high-resolution imaging of the liver, helping to differentiate between benign and cancerous lesions.
AFP Blood Test (Alpha-Fetoprotein)
Elevated levels of AFP may indicate the presence of liver cancer.
PET-CT Scan
Helps determine if liver cancer has spread to other parts of the body.
FibroScan
A non-invasive test to assess the degree of liver scarring and evaluate liver function in patients with liver disease.
Treatment Options
Targeted Therapy and Immunotherapy
- Sorafenib and Lenvatinib: Targeted therapies that block the growth of cancer cells by inhibiting specific proteins and pathways involved in tumor growth.
- Checkpoint Inhibitors (Immunotherapy): Drugs such as nivolumab and pembrolizumab help the immune system recognize and attack cancer cells, often used for advanced liver cancer.
- VEGF Inhibitors: These drugs block the formation of new blood vessels that feed the tumor, slowing its growth.
Chemotherapy and Medical Oncology
- Systemic Chemotherapy: Often used for advanced liver cancer that has spread to other parts of the body, chemotherapy works to shrink tumors and slow their growth.
- Transarterial Chemoembolization (TACE): A minimally invasive procedure where chemotherapy is delivered directly to the liver tumor, along with substances to block the blood supply feeding the tumor.
Radiation Therapy
- Stereotactic Body Radiation Therapy (SBRT): This technique delivers high doses of radiation to the tumor while sparing healthy liver tissue.
- Radioembolization (Yttrium-90 Radioembolization): Tiny radioactive beads are delivered directly into the liver tumor via the bloodstream, targeting cancer cells while minimizing damage to surrounding tissue.
Surgical Treatment
- Liver Resection: Removal of the tumor and a portion of the liver. This is often an option for patients with a single tumor and good liver function.
- Liver Transplantation: In some cases, a liver transplant may be the best option, especially for patients with liver cancer and cirrhosis who are not candidates for liver resection.
- Minimally Invasive Surgery: Laparoscopic techniques allow for smaller incisions and faster recovery times.
Multidisciplinary Approach
Liver cancer treatment requires a highly specialized team of experts working together to provide personalized care. The team includes
- Hepatobiliary Surgeons
- Liver Transplant Surgeons
- Medical Oncologists
- Interventional Radiologists
- Radiation Oncologists
- Gastroenterologists
- Pathologists
- Oncology Nurses
- Palliative Care Specialists
This collaborative approach ensures that every patient receives a treatment plan tailored to their unique condition and needs
Supportive Care and Patient Services
We offer a variety of supportive care services to help patients manage their treatment and maintain their quality of life
Nutritional Counseling
Guidance on maintaining liver health and managing symptoms during liver cancer treatment.
Liver Disease Management
Comprehensive care for patients with cirrhosis, hepatitis, or other chronic liver conditions.
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic liver cancer.
Psychosocial Support
Counseling services for patients and families coping with the emotional and psychological challenges of a liver cancer diagnosis.
Physical Rehabilitation
Post-surgical rehabilitation to help patients recover and regain strength after liver cancer surgery.
Meet Our Experts
We guide liver cancer patients through every step of their journey, from diagnosis to recovery
Patient Journey
Initial Consultation
A thorough evaluation with the liver cancer care team, including diagnostic imaging and tests to assess the extent of the disease.
Personalized Treatment Plan
Based on the patient’s diagnosis, a customized treatment plan is developed, which may include surgery, chemotherapy, radiation, or other approaches.
Treatment and Support
Patients receive comprehensive treatment, supported by our multidisciplinary team of specialists and supportive care services.
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor liver function, assess treatment response, and manage long-term health.









