Head and Neck Cancer

Head and neck cancer refers to a group of cancers that develop in the tissues of the head and neck region, including the throat, larynx, nose, sinuses, and mouth. The most common type is squamous cell carcinoma, which affects the thin, flat cells lining the surfaces of these areas. Early detection and treatment are essential for improving outcomes. At Burjeel Cancer Institute, we provide comprehensive care for head and neck cancers, utilizing surgery, radiation therapy, chemotherapy, and targeted therapies tailored to each patient’s needs.
Symptoms and Risk Factors
- A lump or sore that doesn’t heal
- Persistent sore throat or hoarseness
- Difficulty swallowing
- Ear pain
- Swelling or pain in the jaw
- Unexplained weight loss
- Frequent nosebleeds or nasal congestion
- Pain or numbness in the face
- Persistent cough or trouble breathing

Common Symptoms of Head and Neck Cancer include
Tobacco Use
Smoking cigarettes, cigars, or pipes, as well as chewing tobacco, significantly increases the risk of head and neck cancer.
Alcohol Use
Heavy alcohol consumption, particularly when combined with tobacco use, is a major risk factor.
Human Papillomavirus (HPV)
Infection with certain strains of HPV, particularly HPV-16, is linked to cancers in the oropharynx (the back of the throat, including the tonsils and base of the tongue).
Exposure to Certain Chemicals
Prolonged exposure to asbestos, wood dust, and certain industrial chemicals can increase the risk.
Poor Oral Hygiene
Lack of proper dental care and long-term gum disease may increase the risk of cancers in the mouth and throat.
Family History
A family history of head and neck cancer can increase the risk.
Radiation Exposure
Previous radiation therapy to the head or neck area for other cancers increases the risk.
Risk Factors for head and neck cancer include
We offer a range of advanced diagnostic tools to detect and stage head and neck cancers accurately, including
Physical Examination
A thorough examination of the head and neck region, including the mouth, throat, nose, and lymph nodes, to detect any abnormalities.
Endoscopy
A flexible tube with a camera is used to examine the throat, nasal passages, and voice box for any suspicious areas.
Biopsy
A sample of tissue is taken from the affected area for laboratory analysis to confirm the presence of cancer cells.
CT Scan and MRI
Advanced imaging techniques used to detect tumors, assess their size, and determine whether cancer has spread to nearby structures.
PET-CT Scan
Combines positron emission tomography and computed tomography to detect the spread of cancer to other parts of the body.
Fine Needle Aspiration (FNA)
A minimally invasive procedure used to collect cells from a lump or lymph node for examination under a microscope.
HPV Testing
Testing for the presence of human papillomavirus (HPV), especially in cases of oropharyngeal cancer, to guide treatment decisions.

Diagnostic Procedures
Targeted Therapy and Immunotherapy
- EGFR Inhibitors: Drugs like cetuximab block the epidermal growth factor receptor (EGFR), a protein that promotes the growth of cancer cells, particularly in head and neck squamous cell carcinoma.
- Checkpoint Inhibitors (Immunotherapy): Drugs like pembrolizumab and nivolumab help the immune system recognize and attack cancer cells, often used in cases of recurrent or metastatic head and neck cancer.
Chemotherapy and Medical Oncology
- Systemic Chemotherapy: Used to treat advanced head and neck cancer or when cancer has spread to other parts of the body.
- Concurrent Chemoradiation: Chemotherapy is often combined with radiation therapy to enhance the effectiveness of treatment, particularly for locally advanced cancers.
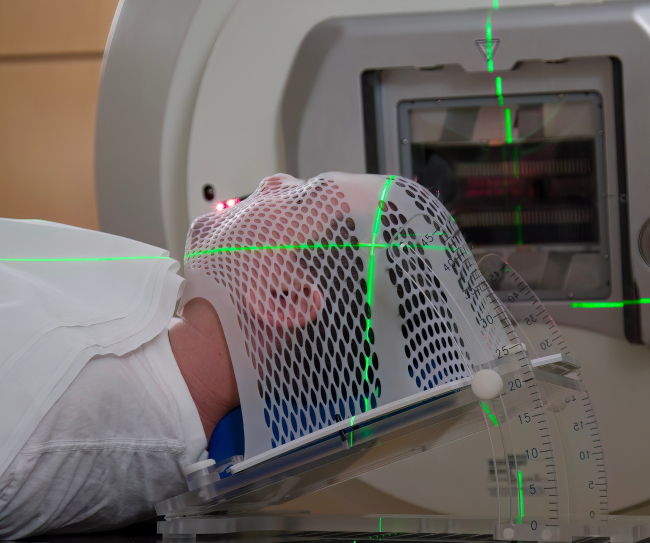
Radiation Therapy:
External Beam Radiation Therapy (EBRT): High-energy radiation is used to target and destroy cancer cells in the head and neck region.
Intensity-Modulated Radiation Therapy (IMRT): A highly precise form of radiation therapy that shapes radiation beams to conform to the tumor, sparing nearby healthy tissues.
Brachytherapy: Internal radiation therapy that delivers radioactive material directly into or near the tumor.
Surgical Treatment
- Tumor Resection: Surgical removal of the tumor, often combined with the removal of surrounding healthy tissue to ensure complete cancer removal.
- Neck Dissection: Removal of lymph nodes in the neck to check for the spread of cancer.
- Reconstructive Surgery: Performed after tumor resection to restore function and appearance, particularly in areas such as the mouth, throat, and jaw.
- Minimally Invasive Surgery: Techniques like transoral robotic surgery (TORS) and endoscopic surgery are used to remove tumors with minimal disruption to surrounding tissues.
Treatment Options
Head and neck cancer treatment at Burjeel Cancer Institute involves a collaborative effort from a multidisciplinary team, including
- Otolaryngologists (ENT Surgeons)
- Medical Oncologists
- Radiation Oncologists
- Reconstructive Surgeons
- Radiologists
- Pathologists
- Speech and Swallow Therapists
- Genetic Counselors
- Oncology Nurses
- Palliative Care Specialists
This approach ensures that every aspect of the patient’s care is covered, from diagnosis to recovery.

Multidisciplinary Approach
We offer a wide range of supportive care services to help patients with head and neck cancer manage their treatment and improve their quality of life
Speech and Swallow Therapy
Specialized therapy to help patients regain speech and swallowing functions after treatment.
Nutritional Counseling
Guidance on maintaining adequate nutrition during treatment, especially for patients with difficulty swallowing or eating.
Rehabilitation Services
Physical therapy and rehabilitation programs to help patients recover function and mobility after surgery or treatment.
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic head and neck cancer.
Psychosocial Support
Counseling services for patients and their families to cope with the emotional and psychological challenges of a cancer diagnosis.
Survivorship Program
Ongoing care and monitoring for patients who have completed treatment, focusing on long-term health and recurrence prevention.
Supportive Care and Patient Services
Our head and neck cancer care team includes specialists in
Meet Our Experts
We guide head and neck cancer patients through every stage of their treatment journey, ensuring personalized care and support
Initial Consultation
A thorough evaluation with the head and neck cancer care team, including diagnostic imaging and tests to assess the extent of the disease.
Personalized Treatment Plan
Based on the patient’s diagnosis, preferences, and overall health, a customized treatment plan is developed.
Treatment and Support
Patients receive comprehensive treatment, supported by a multidisciplinary team and personalized supportive care services.
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor their recovery, assess treatment response, and manage long-term health concerns.






