Cervical Cancer
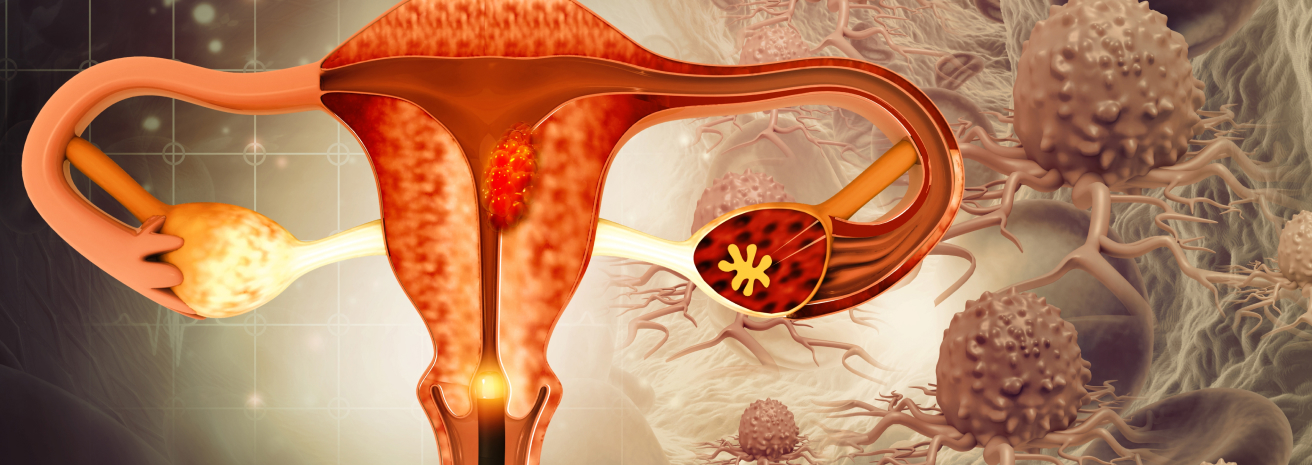
Cervical cancer starts in the cells of the cervix, the lower part of the uterus that connects to the vagina. The majority of cervical cancers are caused by persistent infection with high-risk types of the human papillomavirus (HPV). Early detection through regular Pap smears and HPV testing can prevent the progression of cervical cancer. At Burjeel Cancer Institute, we provide comprehensive care for cervical cancer, including surgery, chemotherapy, radiation therapy, and immunotherapy, with a focus on prevention, early detection, and personalized treatment plans.
Symptoms and Risk Factors
- Abnormal vaginal bleeding (between periods, after intercourse, or after menopause)
- Watery, bloody vaginal discharge
- Pelvic pain or discomfort
- Pain during intercourse
- Urinary or bowel changes in advanced cases
Risk Factors for Cervical Cancer
Human Papillomavirus (HPV)
Infection with high-risk HPV strains is the leading cause of cervical cancer
Sexual History
Early sexual activity, multiple sexual partners, and unprotected intercourse increase the risk of HPV infection
Smoking
Tobacco use weakens the immune system, making it harder for the body to clear HPV infections, increasing the risk of cervical cancer
Weak Immune System
Women with weakened immune systems (due to HIV, for example) have a higher risk of cervical cancer
Family History
A family history of cervical cancer may increase risk
Long-Term Use of Oral Contraceptives
Prolonged use of birth control pills may slightly increase the risk of cervical cancer
Diagnostic Procedures
Common Symptoms of Cervical Cancer include
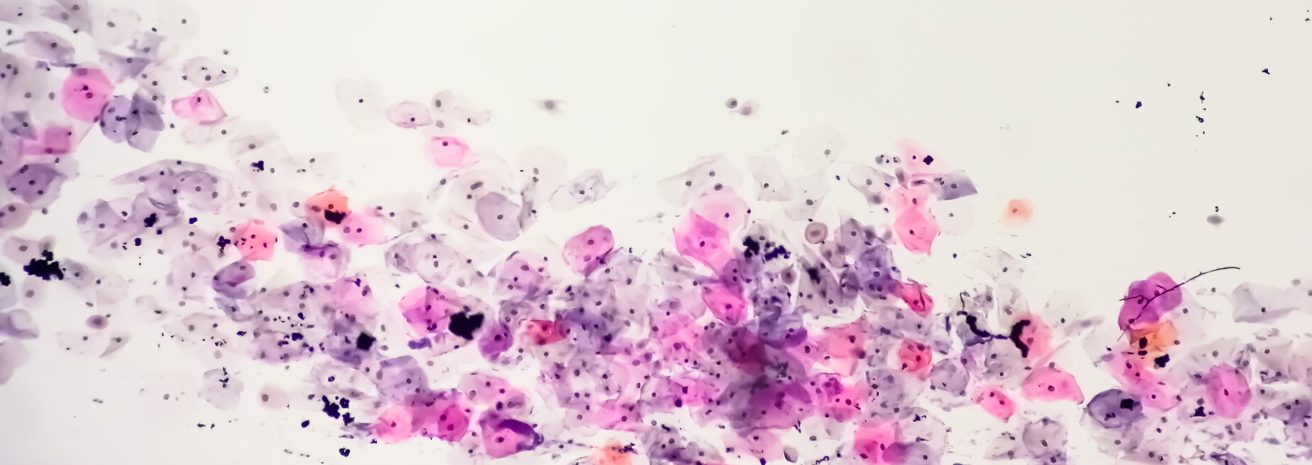
Pap Smear
A screening test that detects precancerous changes in the cervix by collecting cells for microscopic examination
HPV Testing
Identifies the presence of high-risk HPV strains that can lead to cervical cancer
Colposcopy
A diagnostic procedure that uses a magnifying instrument to closely examine the cervix for abnormal areas after an abnormal Pap smear
Cervical Biopsy
Removal of a small sample of tissue from the cervix for laboratory analysis to confirm the presence of cancerous cells
Endocervical Curettage (ECC)
A procedure that removes cells from the endocervical canal for examination, often used when colposcopy results are unclear
CT Scan or MRI
Used to assess the spread of cancer within the pelvis or to other areas of the body
PET-CT Scan
Advanced imaging used to detect metastatic spread of cervical cancer
Treatment Options
Targeted Therapy and Immunotherapy:
- VEGF Inhibitors: Drugs like bevacizumab block the formation of new blood vessels that tumors need to grow, often used in advanced or recurrent cervical cancer.
- Immunotherapy: Drugs that help stimulate the immune system to recognize and destroy cancer cells, offering new hope for patients with advanced or metastatic cervical cancer.
Chemotherapy and Medical Oncology
- Systemic Chemotherapy: Often used in combination with radiation therapy (chemoradiation) to enhance the effectiveness of treatment or as a standalone treatment in advanced cases.
- Combination Chemotherapy: Multiple chemotherapy drugs are used together to target cancer cells more effectively, particularly for metastatic or recurrent cervical cancer.
Radiation Therapy:
- External Beam Radiation Therapy (EBRT): High-energy radiation is delivered to the cervix and surrounding areas to kill cancer cells and shrink tumors.
- Brachytherapy: Internal radiation therapy where radioactive materials are placed directly inside or near the tumor in the cervix, delivering a high dose of radiation with minimal exposure to nearby healthy tissue.
Surgical Treatment
- Conization (Cone Biopsy): Removal of a cone-shaped section of abnormal tissue from the cervix, often used for early-stage or precancerous lesions.
- Hysterectomy: Removal of the uterus and cervix, typically used in early-stage cervical cancer. A radical hysterectomy may include removal of the surrounding tissues, fallopian tubes, and lymph nodes.
- Trachelectomy: Fertility-sparing surgery that removes only the cervix and surrounding tissue while preserving the uterus.
- Pelvic Exenteration: Extensive surgery for advanced cervical cancer that involves the removal of the pelvic organs, including the bladder and rectum, in rare cases.
Multidisciplinary Approach
Early detection of cervical cancer is crucial for effective treatment. We offer a range of diagnostic tools and procedures, including
- Gynecologic Oncologists
- Medical Oncologists
- Radiation Oncologists
- Surgical Oncologists
- Radiologists
- Pathologists
- Genetic Counselors
- Oncology Nurses
- Palliative Care Specialists
This multidisciplinary approach ensures that patients receive personalized care tailored to their individual needs
Supportive Care and Patient Services
Cervical cancer care at Burjeel Cancer Institute is provided by a team of specialists who collaborate to ensure the best possible outcomes for each patient. Our team includes
Nutritional Counseling
Specialized dietary advice to support overall health and manage treatment side effects
Fertility Preservation
Options such as egg freezing or fertility-sparing surgery for women who wish to preserve their fertility before treatment
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic cervical cancer
Psychosocial Support
Counseling services to help patients and families cope with the emotional and psychological challenges of a cervical cancer diagnosis
Physical Rehabilitation
Post-surgical rehabilitation programs to help patients regain strength and function after treatment
Survivorship Program
Ongoing care and monitoring for women who have completed treatment, focusing on recurrence prevention and long-term health
Meet Our Experts
We offer a range of supportive care services to help women with cervical cancer manage their treatment and maintain their quality of life
Patient Journey
We guide cervical cancer patients through every step of their journey, from diagnosis to recovery
Initial Consultation
A thorough evaluation with the gynecologic oncology team, including diagnostic imaging and tests to assess the extent of the disease
Personalized Treatment Plan
A customized treatment plan is developed based on the patient’s diagnosis, cancer stage, and overall health
Treatment and Support
Patients receive comprehensive care, supported by our multidisciplinary team and personalized supportive care services
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor their recovery, assess treatment response, and manage long-term health






