Pancreatic Cancer
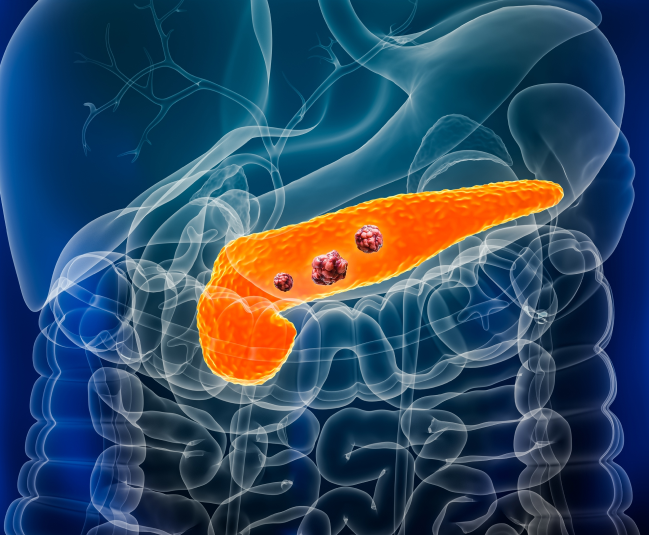
Pancreatic cancer is an aggressive form of cancer that often goes undetected until it is in advanced stages. It arises in the tissues of the pancreas, which plays an important role in digestion and blood sugar regulation. Early diagnosis is challenging, but advances in treatment provide new hope for improved outcomes. At Burjeel Cancer Institute, we offer a comprehensive approach to pancreatic cancer care, including surgery, chemotherapy, radiation therapy, and innovative targeted therapies
Symptoms and Risk Factors
- Unexplained weight loss
- Jaundice (yellowing of the skin and eyes)
- Upper abdominal or back pain
- Loss of appetite
- Nausea and vomiting
- New-onset diabetes or difficulty controlling blood sugar in diabetic patients
- Light-colored stools or dark urine
- Fatigue

Risk Factors for Pancreatic Cancer
Age
Most cases occur in individuals over the age of 60.
Family History
A family history of pancreatic cancer or genetic mutations such as BRCA1, BRCA2, and Lynch syndrome increases the risk.
Chronic Pancreatitis
Long-standing inflammation of the pancreas, often due to alcohol use or genetic conditions, raises the risk.
Diabetes
Individuals with type 2 diabetes or recent-onset diabetes are at higher risk.
Smoking
Tobacco use is a major risk factor for pancreatic cancer.
Obesity
Being overweight or obese can increase the likelihood of developing pancreatic cancer.
Diagnostic Procedures
Pancreatic cancer can be difficult to diagnose early. At Burjeel Cancer Institute, we use advanced diagnostic tools to detect and stage the disease
Endoscopic Ultrasound (EUS)
Combines endoscopy and ultrasound to obtain detailed images of the pancreas and surrounding structures.
CT Scan and MRI
Used to detect tumors, assess their size, and determine if cancer has spread to nearby tissues or organs.
ERCP (Endoscopic Retrograde Cholangiopancreatography)
A procedure used to diagnose and treat conditions in the bile and pancreatic ducts, often helping to relieve jaundice or remove blockages caused by tumors.
PET-CT Scan
A combined imaging technique used to detect cancerous cells and evaluate whether cancer has spread to other areas.
Blood Tests
Tumor markers such as CA 19-9 can sometimes be elevated in people with pancreatic cancer, although they are not definitive.
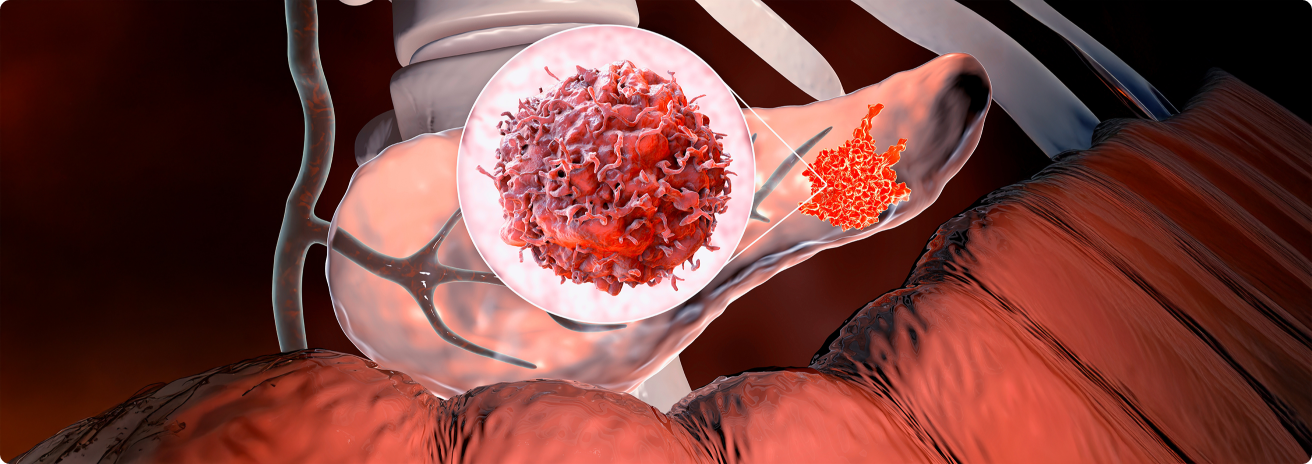
Biopsy
A tissue sample is taken from the pancreas or surrounding area to confirm the presence of cancer cells.
Treatment Options
Targeted Therapy and Immunotherapy
- PARP Inhibitors: For patients with BRCA mutations, targeted therapies such as PARP inhibitors block cancer cells from repairing damaged DNA.
- Immunotherapy (Checkpoint Inhibitors): In certain cases, immunotherapy can help the body’s immune system recognize and destroy pancreatic cancer cells.
- VEGF Inhibitors: These drugs block the formation of new blood vessels that feed tumors, helping to slow their growth.
Chemotherapy and Medical Oncology
- Adjuvant and Neoadjuvant Chemotherapy: Chemotherapy is often given before surgery to shrink tumors or after surgery to destroy any remaining cancer cells.
- Systemic Chemotherapy: For advanced pancreatic cancer, chemotherapy may be used to control the growth of the cancer and improve symptoms.
Radiation Therapy
- External Beam Radiation Therapy (EBRT): Targeted radiation is delivered to the pancreatic tumor to shrink it before surgery or destroy remaining cancer cells after surgery.
- Stereotactic Body Radiation Therapy (SBRT): Delivers high doses of radiation with precision, often used in cases where surgery is not possible.
Surgical Treatment
- Whipple Procedure (Pancreaticoduodenectomy): The most common surgery for pancreatic cancer, involving the removal of the head of the pancreas, part of the small intestine, the gallbladder, and sometimes part of the stomach.
- Distal Pancreatectomy: Removal of the body and tail of the pancreas, often along with the spleen, for tumors located in the tail.
- Total Pancreatectomy: Complete removal of the pancreas, along with surrounding tissues, used in rare cases where the cancer is widespread within the pancreas.
- Minimally Invasive Surgery: Laparoscopic techniques are used in some cases, offering smaller incisions and faster recovery.
Multidisciplinary Approach
Pancreatic cancer care requires the collaboration of a multidisciplinary team that includes
- Hepatobiliary Surgeons
- Medical Oncologists
- Radiation Oncologists
- Gastroenterologists
- Interventional Radiologists
- Pathologists
- Genetic Counselors
- Oncology Nurses
- Palliative Care Specialists
This team works together to develop a personalized treatment plan based on the stage and characteristics of the cancer, as well as the patient’s overall health
Supportive Care and Patient Services
We offer a range of supportive care services to help patients manage pancreatic cancer treatment and maintain their quality of life
Nutrition Counseling
Pancreatic cancer can affect digestion and nutrient absorption, so we offer specialized nutrition plans to support patients during treatment.
Pain Management
Our palliative care team provides effective pain management strategies for patients experiencing discomfort from pancreatic cancer or its treatments.
Psychosocial Support
Counseling services to help patients and families cope with the emotional and psychological challenges of a pancreatic cancer diagnosis.
Physical Rehabilitation
Post-surgical rehabilitation programs designed to help patients regain strength and improve quality of life after treatment.
Palliative Care
Symptom management and quality-of-life support for patients with advanced or metastatic pancreatic cancer.
Patient Journey
We guide pancreatic cancer patients through every stage of their journey, ensuring personalized care and support
Initial Consultation
A thorough evaluation with the pancreatic cancer care team, including diagnostic imaging and tests to assess the extent of the disease.
Personalized Treatment Plan
A customized treatment plan is developed based on the patient’s diagnosis, preferences, and overall health.
Treatment and Support
Patients receive comprehensive treatment, supported by a multidisciplinary team and personalized supportive care services.
Follow-Up Care
After treatment, patients receive regular follow-ups to monitor progress, manage symptoms, and address long-term health concerns.





